Revelations Per Minute Radio Show Discuss Page
Rh Negative Definitions:
Rh-Negative Blood Type:
The blood group whose red cells lack the Rh factor (Rh antigen).Source
The Rh Factor:
Any one or more genetically determined antigens present in the red blood cells of most persons and higher animals & capable of inducing intense immune reactions. Rh antigens were 1st identified in 1939 in Rhesus monkeys.Source
There are four blood types (A, B, AB, and O).
Each of the four blood types is additionally classified according to the presence of another protein on the surface of red blood cells that indicates your Rh factor.
If you carry this protein, you are Rh positive. If you don't carry the protein, you are Rh negative.
When and Why is this important?
The most public mention of Rh-Negative Blood having ANY importance is during Pregnancy. |
|
What does that mean in layman's terms? Basically, the Rh Negative Mother's body, without any medical or scientific intervention; will most likely have a natural immune response that results in the mother's body recognizing the fetus as a foreign object, like an infection or cancer and she will create antibodies that will set out to attack the RBC of the fetus by making them swell with inflammation and then burst...which can lead to serious illness or death of the fetus. |
However, besides pregnancy there are many other times the Rh Negative Factor is important including blood transfusions, plasma transfusions, blood donations, organ transplants, skin grafts and genetic conditions.
Without Science stepping in, Rh-Negatives are genetically predisposed to developing anti-bodies against Rh-Negative blood, flesh or fetus due to a lack of D antigen on the red blood cells.
DNA, Chromosomes, Genes, Proteins & the Rhesus Negative Factor
 The Human Genome Project
The Human Genome Project
Source:  U.S. National Library of Medicine / National Institute for Health
U.S. National Library of Medicine / National Institute for Health
The entire human genome consists of 23 pairs of chromosomes with one chromosome in every pair coming from each parent.
The RHD Gene is Located on Chromosome 1
Cytogenetic Location:
1p36.11
Molecular Location on Chromosome 1: base pairs 25,598,980 to 25,656,935
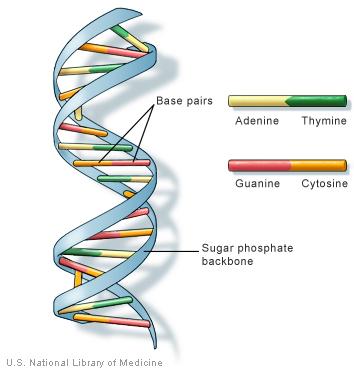
Chromosomes are tightly coiled microscopic structures made up mainly of DNA, which consists of four different building blocks called bases (A, T, C, and G). The information in DNA is stored as a code made up of these four chemical bases: adenine (A), guanine (G), cytosine (C), and thymine (T). The four bases are repeated millions of times to form each chromosome. With few exceptions (e.g., red blood cells), each of the trillions of cells in the human body contains a complete set of chromosomes—the genome. The order, or sequence, of these bases determines the information available for building and maintaining an organism, similar to the way in which letters of the alphabet appear in a certain order to form words & sentences. Genes are chromosome pieces whose base sequence (e.g., ATTCGGA) determines how, when, and where the body makes each of the many thousands of different proteins required for life.
How do genes direct the production of proteins?
Most genes contain the information needed to make functional molecules called proteins.
The journey from gene to protein is complex and tightly controlled within each cell. It consists of two major steps: transcription and translation. Together, transcription and translation are known as gene expression.
During the process of transcription, the information stored in a gene’s DNA is transferred to a similar molecule called RNA (ribonucleic acid) in the cell nucleus. Both RNA and DNA are made up of a chain of nucleotide bases, but they have slightly different chemical properties. The type of RNA that contains the information for making a protein is called messenger RNA (mRNA) because it carries the information, or message, from the DNA out of the nucleus into the cytoplasm.
Translation, the second step in getting from a gene to a protein, takes place in the cytoplasm. The mRNA interacts with a specialized complex called a ribosome, which “reads” the sequence of mRNA bases.
Each sequence of three bases, called a codon, usually codes for one particular amino acid. (Amino acids are the building blocks of proteins.)
A type of RNA called transfer RNA (tRNA) assembles the protein, one amino acid at a time. Protein assembly continues until the ribosome encounters a “stop” codon (a sequence of three bases that does not code for an amino acid).
The flow of information from DNA to RNA to proteins is one of the fundamental principles of molecular biology. It is so important that it is sometimes called the “central dogma.” Through the processes of transcription and translation, information from genes is used to make proteins.
Proteins are large, complex molecules that play many critical roles in the body. They do most of the work in cells and are required for the structure, function, and regulation of the body’s tissues and organs.
Proteins are made up of hundreds or thousands of smaller units called amino acids, which are attached to one another in long chains. There are 20 different types of amino acids that can be combined to make a protein. The sequence of amino acids determines each protein’s unique 3-dimensional structure and its specific function. Proteins are categorized according to their range of functions in the body and include Antibodies, Enzymes, Messenger Proteins, Structural Components and Transport and Storage proteins. Specifically for our conversation, Antibodies bind to specific foreign particles, such as viruses and bacteria, to help protect the body. For more information, click  here.
here.
Proteins, Antigens and the Rhesus Factor
Source:  Wikipedia
Wikipedia
An individual either has, or does not have, the "Rhesus factor" on the surface of their  red blood cells. This term strictly refers only to the most immunogenic D antigen of the Rh blood group system, or the Rh- blood group system.
red blood cells. This term strictly refers only to the most immunogenic D antigen of the Rh blood group system, or the Rh- blood group system.
The status is usually indicated by Rh positive (Rh+ does have the D antigen) or Rh negative (Rh- does not have the D antigen) suffix to the  ABO
ABO  blood type. However, other antigens of this blood group system are also clinically relevant. These antigens are listed separately (see website:
blood type. However, other antigens of this blood group system are also clinically relevant. These antigens are listed separately (see website:  Rh nomenclature). In contrast to the ABO blood group, immunization against Rh can generally only occur through
Rh nomenclature). In contrast to the ABO blood group, immunization against Rh can generally only occur through  blood transfusion or placental exposure during pregnancy.
blood transfusion or placental exposure during pregnancy.
The proteins which carry the Rh antigens are  transmembrane proteins, whose structure suggest that they are
transmembrane proteins, whose structure suggest that they are  ion channels.The main antigens are D, C, E, c and e, which are encoded by two adjacent gene loci, the RHD gene which encodes the RhD protein with the D antigen (and variants)and the RHCE gene which encodes the RhCE protein with the C, E, c and e antigens (and variants). There is no d antigen. Lowercase "d" indicates the absence of the D antigen (the gene is usually deleted or otherwise nonfunctional).
ion channels.The main antigens are D, C, E, c and e, which are encoded by two adjacent gene loci, the RHD gene which encodes the RhD protein with the D antigen (and variants)and the RHCE gene which encodes the RhCE protein with the C, E, c and e antigens (and variants). There is no d antigen. Lowercase "d" indicates the absence of the D antigen (the gene is usually deleted or otherwise nonfunctional).
Rh phenotypes are readily identified by identifying the presence or absence of the Rh surface antigens. Most of the Rh phenotypes can be produced by several different Rh genotypes. The exact genotype of any individual can only be identified by DNA analysis. Regarding patient treatment, only the phenotype is usually of any clinical significance to ensure a patient is not exposed to an antigen they are likely to develop antibodies against. A probable genotype may be speculated on, based on the statistical distributions of genotypes in the patient's place of origin.
Plainly put --- In Rh Negative people the DNA to RNA message is DO NOT create the protein for the Rhesus Factor or D Antigen...the natural DNA message is to create Anti-Bodies to protect itself!
Beyond the Basic ABO Blood Types
Beyond the Rh Factor, numerous other agglutinators have been discovered in addition to the classic ABO blood types, including N and M blood types, Lutheran, Kell, Kidd, Duffy, Lewis and more.
The A antigens fall into two subtypes--A1 and A2. A1 is said to include American Indians, Pacific Islanders, Austroloids, and Asiatics. Rh-negative genes occur in approximately 15% of Europeans. This blood type is virtually absent in Asians, Pacific Islanders, Australians, and American Indians when comparing statistics.
Overview of Phenotype Frequencies
A, B, and O
O is the most common group with over 50% of the population are of this type. B is is almost absent in Australia and aboriginal American, and more common in Europe with around 15%. In Africa, India, and Asia has nearly 40% of the blood type B. A2 is limited to Europe.
Diego
Diego-positive blood types are limited to American Indians and Asians. This blood type is non-existent in Europe, Africa, Micronesia, Australia, Polynesia, and in Eskimos.
Duffy
Most Polynesians and Australians and approximately 95-99% of Asians are Duffy-positive. Indics are 90% Duffy-positive, 90% are American Indians, 65% are populations of America and England, and 27% are Afro-American.
Kidd
Kidd-positive is most common in West Africa and African Americans with greater than 90%. North American Indians are approximately 90% Kidd-positive as well. Europeans are around 70% and least common in in the Chinese at around 50%.
From  Entrez Gene
Entrez Gene![]() :
:
MNS and U
American Indians have almost exclusively M. N occurs most commonly in the Pacific and Australia. MS and NS are absent in Australia. U negative is rare and limited to Africa.
Rh
Rh-negative blood types are rare and absent in most of the world, however approximately 15% of Europeans are Rh-negative.
The Rh blood group system is the second most clinically significant of the blood groups, second only to ABO. It is also the most polymorphic of the blood groups, with variations due to deletions, gene conversions, and missense mutations. The Rh blood group includes this gene, which encodes the RhD protein, and a second gene that encodes both the RhC and RhE antigens on a single polypeptide. The two genes, and a third unrelated gene, are found in a cluster on chromosome 1. The classification of Rh-positive and Rh-negative individuals is determined by the presence or absence of the highly immunogenic RhD protein on the surface of erythrocytes. Multiple transcript variants encoding different isoforms have been found for this gene.
My Story of the Chuck...

If a chicken (Rh++) and a duck (Rh- -) try to mate, they do NOT create a CHUCK (Rh+/-) naturally....BUT if there was already an animal that was a CHUCK (Rh+/-) it would have an easier time mating with both the chick (Rh++) and the duck (Rh- -), because it is 1/2 of what it is trying to mate with... I think the confusion in the body of the "CHUCK" (Rh+/-) creates a "dis-eased" condition in the body via the immune system.
I also think the Rh- vs Rh+ stats have to be more like 15-20% Rh-, 25-30% RH+ and the rest 50-60% Rh+/- in the United States, thus recognizing the recessive carriers are their own sub category; as they are neither Rh+ or Rh- but BOTH...they are Chucks!
Hope this helps you understand how I began down this road of research. My parents, siblings and children are all CHUCKS (Rh+/-) .... I am the only rare DUCK! (Rh-/-)
Rh-Negative are not taught to know just how different we are!
We are told that there is no medical importance to our general health, unless pregnant or in need of a donor
Here is some information about the HLA-B27 genetic marker that runs positive in my family for generations. This explains the reasoning for testing both the RH- Status of your blood and the HLA-B27 Genetic Marker if you have Undiagnosed Pain or Joint Issues or have an Autoimmune Disease.
Ankylosing Spondylitis and Rheumatoid Arthritis are just two of many autoimmune disease that may be more prevalent to those people who are tested positive for a genetic marker called HLA-B27 and which tend to lap over each other making for hard diagnosing of the conditions.
 My theory that the Rh-Negative & Recessive Blood Factors are associated with HLA-B27 positive genetic marker readings, is based on the research that 85+% of individuals diagnosed with Ankylosing Spondylitis or "AS"; happen to test positive for the HLA-B27 genetic marker, which is said to be had by only about 8% of the population or less, based on geographical location. I saw a connection because the blood type O- also appears in about 7% of the population and again that percentage varies by the geographical location of the population. After researching this connection and family history, I felt confidant enough to lay out my theory for my mothers' doctors, they listened and tested her for the genetic marker and it came back positive, as did mine, my children's and my grandmother's. Again this is a genetic marker that supposedly only 8% of the world carry.
My theory that the Rh-Negative & Recessive Blood Factors are associated with HLA-B27 positive genetic marker readings, is based on the research that 85+% of individuals diagnosed with Ankylosing Spondylitis or "AS"; happen to test positive for the HLA-B27 genetic marker, which is said to be had by only about 8% of the population or less, based on geographical location. I saw a connection because the blood type O- also appears in about 7% of the population and again that percentage varies by the geographical location of the population. After researching this connection and family history, I felt confidant enough to lay out my theory for my mothers' doctors, they listened and tested her for the genetic marker and it came back positive, as did mine, my children's and my grandmother's. Again this is a genetic marker that supposedly only 8% of the world carry.
You do not need to be Rh-Negative to come from an Rh- Blood line...You can be like me. I am 1 of 11 kids in my family and I am the only Rh- but my parents are both 1/2 breeds (Rh+/-) meaning that they have an Rh- RECESSIVE blood factor. Some interesting information.
1.) The HLA-B27 genetic marker is said to be had by approx. 8% of the world's population. Similarly Type O- blood is had by about 7% of the world. Both share traits that show their migration pattern through geographical location & ethnic background, nearly hand in hand.
2.) Rh- (- -) and Rh+ (+ +) people have different immune systems. Rh-Negative people have a stronger immune system response. Medical professional's don't even acknowledge those who are Rh (+ -) and the implications it may have on their individual immune system type.
3.) Copper and Inflammation - Copper in an important factor in the body's immune response. It is said that Rh- people are more cooper based and Rh+ people are more iron based. Since Auto immune diseases like AS can cause inflammation, I believe copper levels should be looked at more seriously, especially in relationship to the natural levels for that persons specific blood type. If iron is taken so seriously with anemia, why not look at the connection to copper, inflammation and neuropathy that so many of us complain of.
4.) We process CO2 more efficiently.
5.) We have Vitamin and Mineral Absorption Issues. Especially Vitamin D, B12, B6 and sometimes K, as well as Iron, Zinc and Copper Influxes and Imbalances.
There are other clues I used to put my theory together. So far, I have proven it correct in my family. My mother's doctors never tested her for HLA-B27 or autoimmune until I approached them with this information. It was enough to make them take a look at it as a possibility and she was positive. My mother is HLA-B27+ and blood type O+, but she is really blood type OO+ - and to simplify it, her blood type becomes O+. So while she is Rh+... she is also Rh-. If this is not a true statement, she cannot be my mother.
I am type AO - - = Type A-
My hubby OO - + = Type O+
Child 1 is AO - + = Type A+
Child 2 is OO - + = Type O+
I also believe that the disease manifests itself differently in symptom based on this theory, as it seems Rh- and Rh+ people show the predominance of certain issues and symptoms as a group. Meaning more Rh+ people have issues A,B,& C while Rh- people experience more of D, E, & F. I believe it would be much easier to see these trends with less confusion if there were 12 blood type classifications; instead of the basic 8 recognized (shown in red) .
Over time we've been given the almost unchanging US statistics of: 15% are Rh- and 85% are Rh+
First of all, most people do not know their blood type...so where does this statistic come from???
If your 2 blood factors are - - they call you Rh-
If your 2 blood factors are ++ they call you Rh+
If your 2 blood factors are + - they still call your Rh+ and YOU ARE NOT.
You'd be a half breed :) 1/2 Rh+ and Rh-. If Rh+ are built one way and Rh- are built a completely different way...What about the person in the middle; The Rh+/- People? They must be different as well. Our immune systems, transfer systems, protein production, oxygen & carbon dioxide levels, iron & copper levels & more!
Rh-Positive Types: A+, B+, AB+ & O+
Rh-Negative Types: A-, B-. AB- & O-
Rh-Neutral Types: A+/-, B+/-, AB+/- & O+/-
If you have ever researched your Rh-Negative blood, I'm sure you have probably seen the many popular lists online about the "Rh-Negative Shared Traits". I've decided to compiled a NEW List of the "Shared Rh-Negative Traits"; but this time looking at things from a different angle, one which may actually explain some of these shared traits.
Please note, some of the traits are not accounted for on both of the lists. These lists should not be used for anything but entertainment, as I cannot prove either of them to be 100% true of everyone; rather they are compiled of the many accepted public opinions and research studies.. These list are not, at all meant to be used as a diagnostic tool. If you have any health concerns, you should consult your doctor for advice.
The Existing ListA feeling of not belonging >>>> Sense of a "Mission" in life >>>> Compassion for Mankind >>>> An extra rib or vertebra >>>> Higher than average IQ >>>> Sensitive vision & senses >>>> Lower body temperature >>>> Blue, green, Hazel eyes >>>> Red/reddish tint to hair >>>> Heat & Sunlight Sensitivity >>>> Tend to be Healers >>>> Empathetic Illnesses >>>> Unexplained phenomenon >>>> Physic Dreams and/or Ability >>>> Higher blood pressure (some say lower) >>>> Truth seekers >>>> ESP Ability >>>> Love of Space & Science >>>> Cannot be cloned >>>> Unexplained Scares >>>> Piercing Eyes >>>> Ability to disrupt electrical devices >>>> Prone to Alien Abductions >>>> | A New Twist on the Old ListDepression, Antisocial Personality Disorder Obsessive Compulsive Disorder (OCD)  INFP Personality INFP Personality Ankylosing Spondylitis Asperger's Syndrome Glaucoma & Photophobia Secondary Hypothermia OCA2 gene Neandertal Origin, Melanocortin 1 Receptor (MC1R), Pheomelanin, Melanoma Lupus, Melanin Issue High Natural Copper Levels  INFP Personality INFP PersonalityAn Over-Active Immune System Sleep Disorders Sleep Apnea, Narcolepsy Increased Risk of Autoimmune Disease Related Heart Conditions |
Ankylosing spondylitis in the pharaohs of ancient Egypt.
BACKGROUND: Among the pharaohs of the 18th and 19th dynasty of Old Egypt, at least three had ankylosing spondylitis: Amenhotep (Amenophis) II, Ramses II ("The Great"), and his son Merenptah. OBJECTIVE: An illustrated review is given on the radiological indications for their disease, together with the rough history of these pharaohs, the history of their tombs, of the detection of their mummies in the 19th century and of their paleopathological investigation.
About King Tut
Boyer's closer re-examination of the 1968 X-rays revealed an abnormal curvature of the spine and fusion of the upper vertebrae. This is a condition associated with scoliosis and a rare disorder called Klippel-Feil syndrome, which makes sufferers look as if they have a short neck. The disorder, which is also associated with anomalies of the kidneys, heart and nervous system, could have left King Tut very fragile and at risk of fatal spinal cord injury from a simple push or a minor fall. Read the full article,  click here.
click here.
First questions: I want to talk about the Shroud of Turin and vaccinations for a moment. There is public dispute on the blood on the Shroud of Turin's DNA/Blood test results. They say the blood was male and Type AB. However, they do not disclose the Rh Factor. This  article states,"This blood type is rare (3.2% of the world population, according to Dr. Leoncio Garza-Valdes of the University of Texas Health Science Center)" which may include the Rh-Negative Type AB people.
article states,"This blood type is rare (3.2% of the world population, according to Dr. Leoncio Garza-Valdes of the University of Texas Health Science Center)" which may include the Rh-Negative Type AB people.
If we are to assume our Creator is of a higher education and knowledge and we now know about vaccinations, immune response and antibodies; would it not make sense that a person being sent to Earth, if it is a foreign place to them; may have been "vaccinated" to protect themselves from the environment? There are studies that individually research the oldest blood type on the planet, which most agree is Type O and studies on the Shroud of Turin which dispute the blood and the person of origin, but which so far have concluded in the blood being Type AB.
Here is my question. Is it possible that the original beings on this planet were Type O, as they were made for the environment and would not need to develop any antigens to defend itself from the environment. Yet a visitor to this planet might assume the need to protect itself against potential infection or exposure? We currently run this practice every single day with infant, travelers and the military.
If we are to assume our Creator is of a higher education and knowledge and we now know about vaccinations, immune response and antibodies; would it not make sense that a person being sent to Earth, if it is a foreign place to them; may have been "vaccinated" to protect themselves from the environment? There are studies that individually research the oldest blood type on the planet, which most agree is Type O and studies on the Shroud of Turin which dispute the blood and the person of origin, but which so far have concluded in the blood being Type AB.
Here is my question. Is it possible that the original beings on this planet were Type O, as they were made for the environment and would not need to develop any antigens to defend itself from the environment. Yet a visitor to this planet might assume the need to protect itself against potential infection or exposure? We currently run this practice every single day with infant, travelers and the military.
Next question: In the conversation of blood typing, Rh-Negative people are a minority with a statistic of 15% or less of the population. Considering this, do you think it is more likely that this trait which is recessive by nature has been bred into the population or that it has been slowly bred out of the general population? Why do you think the statistics of Rh-Negatives and Rh-Positives has not really changed much in almost 100 years?
